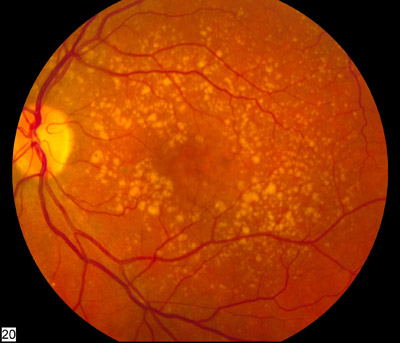
 Macula degeneration (AMD) is a condition that affects the central part of the vision. The part we use to look at things directly. It can occur gradually (dry type) or suddenly (wet type).
Macula degeneration (AMD) is a condition that affects the central part of the vision. The part we use to look at things directly. It can occur gradually (dry type) or suddenly (wet type).
Key facts:
- Mainly affects people over 60, but can occur sooner.
- Most common cause of sight loss in the developed world
- 600,000 people affected in the UK
- Half of these are registered as sight impaired
Risk factors:
- Age – Over 60s at greater risk
- Smoking – Can occur at an earlier age due to smoking
- Genetics – family history increases the risk
- Diet – poor diet can cause deficiencies in the vitamins, mineral and antioxidants needed to main a healthy macula
- Blood pressure – high blood pressure increase the risk
- Sunlight – light from the blue end of the visual spectrum can increase oxidative damage, leading to macula degeneration.
- Gender – women have a greater risk of developing the condition
Risk factor often occur in combination and it is not possible to pin the condition down to one reason or another.
What can i do:
- Having regular eye checks will help pick up the condition sooner, and may even be before you experience any symptoms.
- Look at your lifestyle, take regular exercise, quit smoking, have a diet rich in green leafy vegetables.
- Assessing your lifestyle with your Optometrist can identify areas that may place you at higher risk.
- Taking macula antioxidants if you have risk factors may help to maintain macula health.
- Using good quality sunglasses will help protect your eyes form harmful UV light.
Treatment:
Wet macula degeneration can be treated with a drug that limits the growth of new and leaky blood vessels.
Dry macula degeneration does not have any know treatment however antioxidants are thought to play a part in maintaning macula health and may delay the onset or progression of the condition.
If you will need to be referred, we are able to refer you for wet macula degeneneration by direct fast referral to the following treatment centres.
Meso-Zeaxanthin is only found in one place in the body, the centre of the macula, in the back of the eye. The Meso-Zeaxanthin in MacuShield is extracted from marigolds. These marigolds are grown specifically for the production of of this ingredient. Other sources of Zeaxanthin are certain types of sea food in limited quantities.






